Government
News and insights to help government IT professionals improve public services as well as help businesses understand how law and policy impacts their IT strategy. Coverage includes government support for IT innovations, examinations of regulations and policymaking that businesses may have to adhere to, motivations behind public and private positions on technology, and the approach government agencies take regarding data, commerce, consumer protections, and privacy.
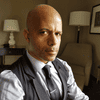
Deepfake and AI artificial intelligence video editing technology. Face of a person in editor. Machine learning concept. Fraud picture swap.
IT Sectors
FTC’s Impersonation Rule and the Fight Against AI-Powered FraudFTC’s Impersonation Rule and the Fight Against AI-Powered Fraud
With AI making fraud easier, the commission responds with a rule to fight the impersonation of government and business.
Never Miss a Beat: Get a snapshot of the issues affecting the IT industry straight to your inbox.

.jpg?width=700&auto=webp&quality=80&disable=upscale)