How GIS Data Can Help Fix Vaccine Distribution
Esri Chief Medical Officer Este Geraghty explains how geographic data and maps can streamline COVID-19 vaccine distribution planning.
Chances are you know someone who has received a COVID-19 vaccine. About one in 10 Americans have been vaccinated so far. But as 50 states with 50 different plans scramble to get their populations vaccinated against the novel coronavirus, the race is on for the US to get to a point where all the people who want a shot get a shot.
Any effort of this magnitude is bound to run into logistical and execution challenges along the way. How do you allocate the correct number of doses to each state and to each facility delivering vaccines? How many workers do you need to administer the shots? How far do people have to travel to receive shots?
Another necessary factor that complicates vaccine delivery is that the US is phasing its approach, vaccinating healthcare workers and essential employees and older citizens first. Vaccines are being administered at veterans’ services centers, state sites, hospitals, and many other venues. The government is working to establish a retail pharmacy vaccination program. It's a complex delivery system.
From the citizen side, there are many stories about people searching out shots, signing up for appointments, and scrambling to get in line for what remains a tight supply of shots. It's been so challenging that there is more than one instance of private citizens or organizations creating their own apps to help people find shots.
It's a challenging undertaking. Is there a way that IT organizations could help? With that question in mind, InformationWeek recently spoke with the Este Geraghty, Chief Medical Officer of geographic information systems company Esri, about how data and more specifically geographic data could contribute to a successful vaccination program rollout of this magnitude. The following is an excerpt of that conversation, edited for this format.

Este Geraghty, Esri
What are the challenges in vaccinating the whole country? How are we doing?
Over time the process does seem to be improving. That's encouraging, but it's been a rocky road.
This is the biggest undertaking in terms of vaccinating a global population that we've ever seen. I mean, certainly polio vaccination is a global endeavor as well, but that's been occurring over decades. So trying to do this in the space of a short period of time for the world and specifically US -- we knew would be challenging. But I think in some ways we've created some of our own challenges.
How so?
There has been so much focus on the process, which is very much what public health professionals do. We're very analytical, and we try to make sure that everything is done correctly.
But in this case, in my opinion, we should be focusing on the outcome. We need to vaccinate the population. How quickly are we going to do it? How many vaccines are we going to endeavor to give per day or per week or per month? What is our timeline for trying to get through this pandemic?
How could organizations use data and GIS to get to that outcome more efficiently? How would you do the vaccine roll out if you were in charge?
Well, obviously hindsight is 2020. I think we can all be really clear that healthcare workers needed to be vaccinated first.
Then I would probably work from age cohorts, depending on vaccine availability, so relatively consistent with the current plans.
But I would be thinking about this with the end goal in mind: The Biden administration's stated goal was 100 million vaccines in 100 days. I would start by trying to allocate vaccines based on the population of each state.
Do you have an example?
I can give you a very good example [with some demo data] for the state of Georgia. You need to do 32,000 vaccines per day to cover your share of the population to make a million vaccines a day to get to 100 million in 100 days, right? To figure out how to do that you work backwards from the goal.
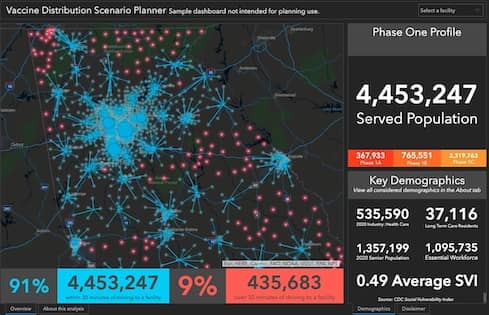
If you look at the state of Georgia, (and a visualization of population locations) it becomes really immediately clear where population centers are and where you have lesser populations. This is a very geographic problem. The Atlanta area has huge populations that will need to be vaccinated. And you have other large cities here and there, but a lot of populations that are not hugely dense, too.
The next thing that I would suggest that we do is look at this geographically. In this map of Georgia, I've aggregated all of those populations to census tracts. Then I'm looking at a visualization of all of the vaccine venues for the state. Then I can calculate the drive time to each of those vaccine venues. I can see if populations have a 30-minute drive time access to vaccine venue, which maybe is my cut off. Or maybe I want it to be a 15-minute walk time or an hour, whatever you want as possible to calculate.
By looking at a map, I can see areas that don't have 30-minute access. If I were taking the (age-based and other) phasing out of the vaccination plans and just focusing on geography, then I would want to work with these areas to make sure these populations have access.
That also solves a geographic equity problem, too.
How do you work on geographic equity?
To work on geographic equity, I can subtract out all the people who already have good access and look at those who don't. And then I can do a number of things. That's where you really have to think about how to manage resources to provide equitable access to vaccines. Maybe you found an empty lot or warehouse that people can drive through.
But now that I've got this visualized on a map, I can adjust it and plan for 20 miles instead. I don't think anybody should have to go further than that. And because I already did the work of mapping the population, I can tell you how many people in my different phases would now have access through those venues.
Having every Starbucks location and every Costco become a vaccine venue is not the key to solving this. The key is having the right number of vaccine venues in the right places so that everybody has access that needs it.
How do we decide on new vaccine venues? They're not all going to be drive-through clinics, right? You might look at retail pharmacies like Walgreens. Or you could look at federally qualified or other health centers that maybe have applied through the national or state system to say I would like to be a provider.

Image: Esri
Once we've optimized the map so that everybody in the state has 30-minute drive time access, I can also look at data for each of these venues and see how many lines of service they're planning to have. How long will it take to deliver each vaccine on average? Then I can calculate what their likely daily vaccination rate will be.
From this view I can see that I can deliver 25,000 vaccines with all of my nicely spaced venues, but I don't have enough capacity to deliver enough vaccines per day.
This is a human resource problem.
At first glance we would say, oh, yeah, Georgia's very well covered because everybody has 30-minute access. But in actuality, they don't have enough people working the venues in Atlanta to make them as useful as they could be.
In that case it could be more financially sound and faster to increase the workforce in the existing sites that already provide access than to simply keep creating new sites.
That's what you mean by focusing on the outcome we want rather than the process?
This is what I'm talking about? Reverse engineering the problem to work to an actual goal that will get us to vaccinated and to herd immunity in the fastest possible way.
The faster we can get this vaccine out to everybody in the US and globally, the better off we're all going to be and the more effective our current efforts will be because those new strains that are highly transmissible can really throw a wrench in the works.
Read more about data and analytics here:
How Data, Analytics & AI Shaped 2020, and Will Impact 2021
A Question for 2021: Where’s My Data?
How to Create a Successful AI Program
Analytics Salaries Steady Amid COVID Crisis
About the Author(s)
You May Also Like
How to Amplify DevOps with DevSecOps
May 22, 2024Generative AI: Use Cases and Risks in 2024
May 29, 2024Smart Service Management
June 4, 2024







