Digitizing Healthcare On The State Level
A state initiative spurs digital healthcare innovation, blurring the lines between healthcare and human services.
The immediacy, accessibility, and personalization of digital interactions have changed people's behaviors and expectations in many aspects of their lives, and healthcare is no exception.
Digital is making an impact at every level of the healthcare system. It is transforming traditional patient-provider relationships by enabling capabilities such as self-management, healthcare literacy, and remote monitoring -- allowing people to be more proactive and accountable for their well-being. In public health, digital tools are beginning to connect people to medical and human services professionals in profound ways, going beyond traditional interactions with healthcare delivery to address social and behavioral determinants of health.
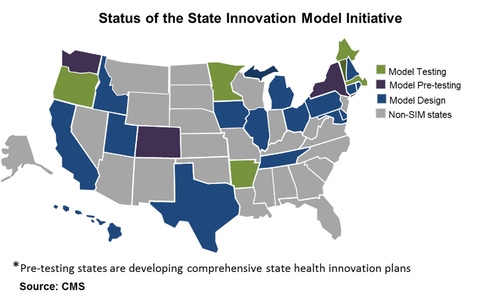
At a state level, the Centers for Medicare and Medicaid Services (CMS) has created a $1 billion initiative to fund participating "State Health Innovation Plans," which aim to improve delivery systems and payment models across Medicare, Medicaid, and the Children's Health Insurance Program. The program awarded 25 states with the first round of funding in 2013 to design models or test improvements. A second round of funding was announced in May 2013.
Historically, health and human services organizations have evolved in silos due to a combination of regulation and categorical funding, but the emergence of these state initiatives is expected to spur some movement. For example, integrating more aspects of health and human service domains, starting with the data they gather and the outcomes they achieve, will break down data silos while making information and operations more transparent and coordinated. That will make the most of community-based assets in the public, private, and nonprofit sectors, and it will align federal resources to eliminate gaps and redundancies.
[Fitness wearables show no sign of slowing down. Read Jawbone's 2 New Fitness Trackers.]
Amplified by the evolving shift from volume to value, state health innovation plans are focusing on integrated and whole-person care, expanded access, population health, and progression toward policies for effective outcomes, according to a new report by Accenture.
Here are the top five investments being made by the 25 state programs.
1. Patient-centered medical homes
All 25 states are investing in or upgrading patient-centered medical homes in order to strengthen primary care integration with specialists and community health workers. An estimated 85% of these will integrate physical and behavioral care. For example, the New York Department of Health is implementing a statewide primary care model that will integrate with behavioral healthcare services and implement a state prevention agenda.
2. All payer claims database (APCD)
States recognize the importance of improved decision making. An estimated 14 states are exploring statewide data aggregation and analytics solutions to reduce redundancy and improve population insights. States are also integrating their health data and their human services program data, enabling them to view people and families more holistically and design more effective program interventions. Accenture's analysis shows that 11 states are investing in population analytics and integrating clinical and public health data. There is also a move to integrate public health data to ensure public health efforts are aligned with care delivery.
3. Lower-cost labor models
All 25 states are aiming to invest in low-cost, community health workers to shift labor costs to more appropriate resources. For example, Maryland is engaging human services navigators as liaisons between primary care coordinators and social services programs. Michigan is developing a collective impact model that engages cross-sector partners, such as businesses and community organizations, to develop health and wellness initiatives.
4. Self-service tools
Fifteen states are equipping consumers with patient portals and other tools to reduce administrative costs while improving self-care. Connecticut, for example, has a website that provides people with the information they need to access community health services. Delaware will commission mobile apps that will allow people to access their personal electronic health records for information on value-based health choices and access to care delivery options.
5. Telehealth
Nineteen states are expected to use virtual care technology, such as telehealth or remote monitoring, to enable more patients to receive care without having to increase the number of healthcare resources. States also are focusing on improving reporting and evaluation to enhance data quality. Some are using geographic information systems (GIS) to match community supports to hotspots of chronic disease burden. Pennsylvania plans to use GIS to enhance surveillance of chronic disease to support evidence-based decision making, overlaying data from multiple sources for an improved view of disease burden and risk factors.
States are exploring new ways of delivering person-centered care and services that will dramatically change care delivery, yet there is a great deal of work still to be done in implementing and scaling states' emerging strategies. Even so, the consensus on the importance of health and human services convergence and person-centered care, which is already happening in local hotspots nationwide, is a promising sign of good things to come.
See the full report by Accenture for more information.
The owners of electronic health records aren't necessarily the patients. How much control should they have? Get the new Who Owns Patient Data? issue of InformationWeek Healthcare today.
About the Author(s)
You May Also Like
How to Amplify DevOps with DevSecOps
May 22, 2024Generative AI: Use Cases and Risks in 2024
May 29, 2024Smart Service Management
June 4, 2024







